Future-Proof Your Revenue Cycle. Today. Accelerate Cash Flow at Scale
RethinkBH Billing unites scheduling, clinical, and financial data in one connected workflow. Automate claims, reduce denials, and accelerate payments within an AI-powered platform built to simplify today and scale for tomorrow.

Smarter Billing, Stronger Results
As ABA practices expand, billing quickly becomes more complex. Multiple payor rules, manual re-entry, and disconnected systems can lead to revenue loss, denials, and compliance issues. RethinkBH Billing automatically generates claims from session data, helping teams submit accurately, reduce risk, and speed up payments.
Fewer manual steps mean fewer headaches – and more time for care.
Predictable Cash Flow,
Without Chaos
Most billing tools stop at submission. RethinkBH Billing keeps revenue moving for high-volume, complex operations with real-time claim tracking visibility, automatic ERA posting, and built-in invoicing connected to your clinical operations.
Claims flow from sessions, payments post automatically, and A/R stays current, all within a secure, enterprise-ready platform designed to empower teams of every size.
Confidence in Every Claim
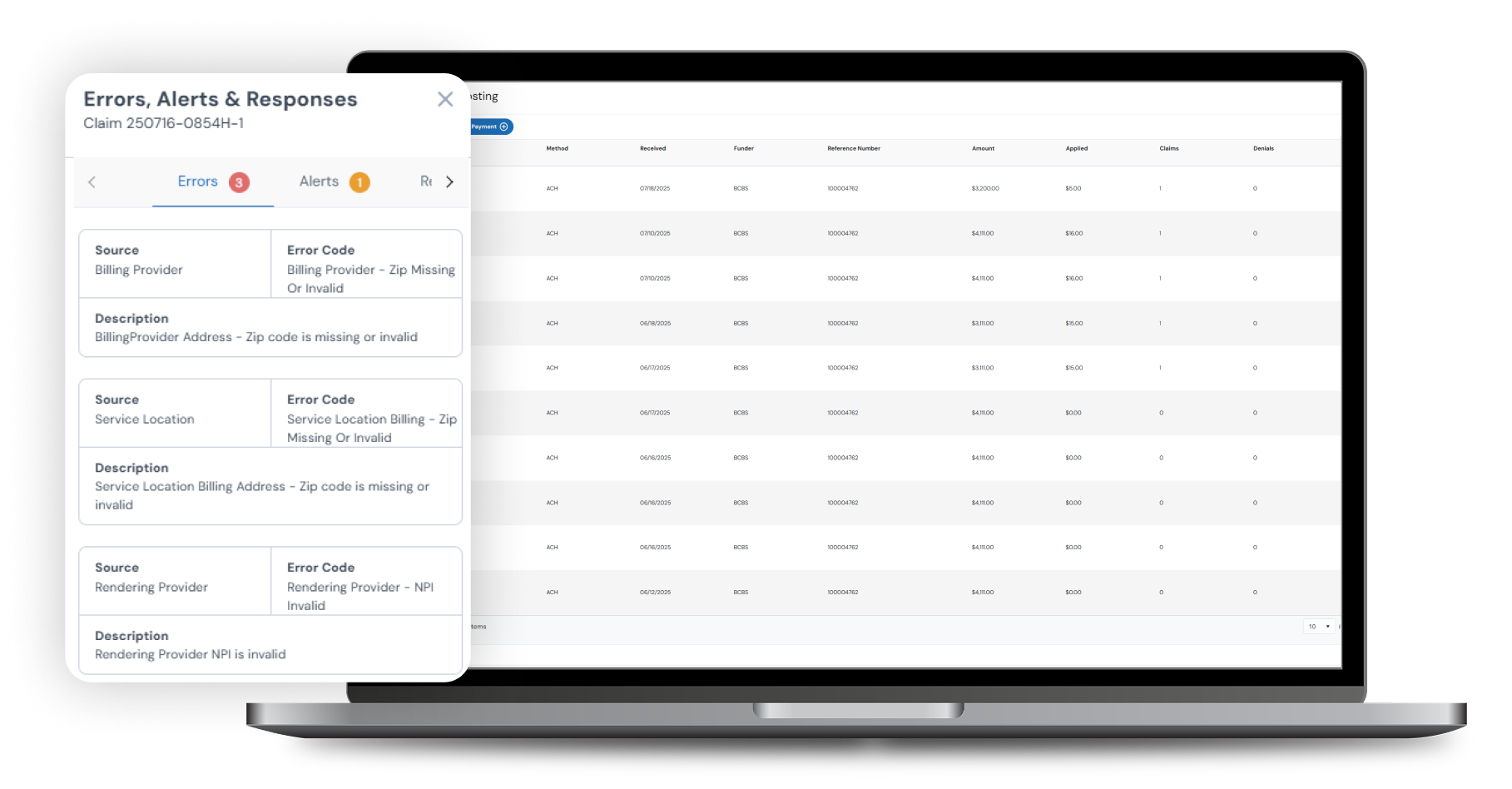
As your organization grows, billing errors can quietly drain productivity and peace of mind. Workflows powered by AI-driven validations, payor-specific rules, and HIPAA-certified security stop issues before they start, keeping revenue steady and teams focused on care.
The result: Audit-ready claims and reliable revenue that help your organization expand, innovate, and lead.
Billing without the Bottlenecks
- Generate clean claims from session data to eliminate duplicate entry.
- Reduce denials with real-time validation before submission.
- Automate payment posting with ERA uploads that reconcile in seconds.
- Improve cash flow with faster reimbursements and complete financial visibility.

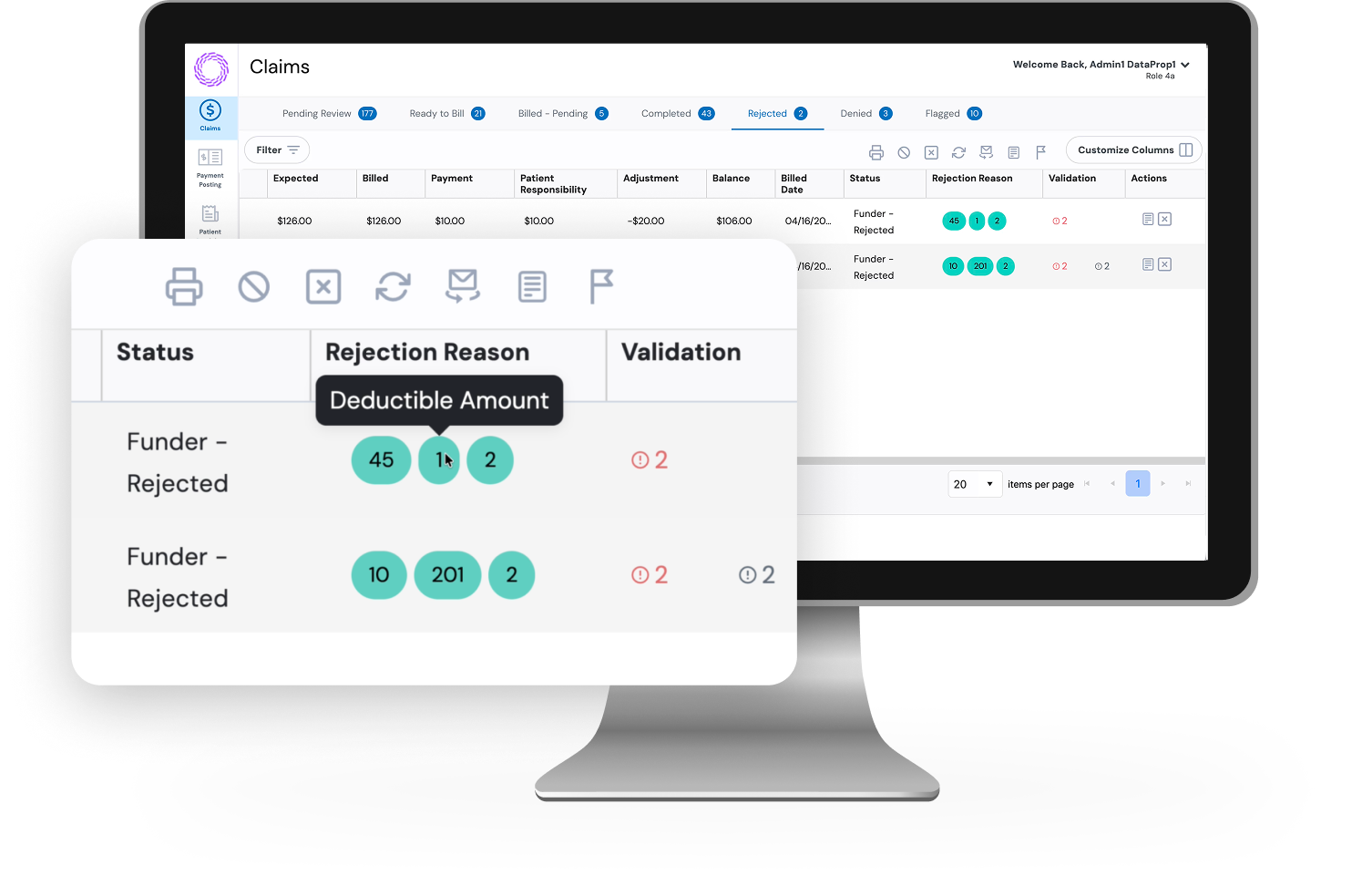
Prevent Denials Before They Happen
Claim rejections are one of the biggest causes of delayed payments. RethinkBH Billing eliminates that risk with intelligent payor rule validations that flag issues before submission so your team can submit clean claims the first time and keep revenue moving.
Faster Payments, Less Paperwork
Many ABA organizations wait 30 to 45 days for reimbursement. RethinkBH Billing shortens that cycle by connecting every step. Claims generate directly from sessions, ERAs post automatically, and balances update instantly – all within a unified, powerful platform.
Built for Growing ABA Practices
RethinkBH Billing is designed to give growing ABA organizations a decisive operational and financial edge. As RethinkBH continues to evolve, we’ll keep advancing the tools and support that practices like yours need to work smarter and scale faster.
Frequently Asked Questions
RethinkBH Billing is an advanced revenue cycle management solution Integrated with the RethinkBH platform. It helps to unify scheduling, clinical documentation, and financial workflows into one system, empowering large ABA organizations to significantly reduce denials, accelerate cash flow, and minimize administrative burden.
It is engineered for ambitious enterprise and multi-site ABA organizations that need to standardize billing, improve revenue predictability, and drive efficiency across complex, high-volume operations.
While most billing platforms are bolted on, RethinkBH Billing is woven in. Claims are generated automatically from the clinical data your team already captures. This real-time, seamless data flow from session to payment is our fundamental differentiator and your greatest advantage.
RethinkBH offers centralized command over billing operations across all your locations, supported by enterprise-grade security and granular, role-based permissions. Our platform is built to master high claim volumes and complex, multi-state payor landscapes, ensuring consistency and compliance as you expand.
Yes. RethinkBH Billing manages the entire process, from insurance claim submission to a complete client invoicing workflow. It tracks client balances and allows you to process payments directly within the system.
Our built-in validation engine cross-references claims against a deep library of payor-specific rules before submission, catching errors that cause denials.
Absolutely. RethinkBH is built on a SOC 2 Type II certified infrastructure and features HIPAA-grade security, comprehensive audit trails, and powerful compliance tools to ensure your data is protected, and your operations are always audit-ready.
Payments can be processed electronically via Electronic Remittance Advice (ERA) files for fully automated reconciliation. The system intelligently matches payments to claims, posts adjustments, and updates balances in real time. Manual payment posting is also fully supported for flexibility.
Yes. Our direct clearinghouse integration provides automated, real-time status updates within the system. Your team can see payor responses and rejection reasons instantly in one place.
RethinkBH provides a strategic partnership, not just support. You will have dedicated implementation resources, tailored training, and ongoing collaboration to ensure your revenue cycle is continuously optimized to meet your strategic goals.
Is Your Billing Holding Back Growth?
Discover How RethinkBH Billing Can Accelerate Revenue at Scale.
Related Resources
Data is crucial in shaping the strategies that define exceptional ABA therapy. Applied Behavior Analysis...
About this ABA Practice Management Guide As an ABA therapy practice owner or clinical director,...
This piece is based on our recent webinar presented by Sarah Schmitz, the Owner and...


